Lactation and the
Transsexual Woman
Additional chapters in This Section include:
Gender Reassignment Surgery
Orchiectomy for MTF Transsexual Women
FFS Facial Feminization Surgery
MTF Transsexual Surgeries
Hormone Replacement Therapy for Transgender Women
Female Hormone Therapy MTF Transsexuals
Breast Development in MTF Transsexuals
MTF Transsexual Breast Enlargement
Breast Augmentation MTF Transsexuals
Lactation and the Transsexual Woman
Injecting Silicone for Transsexual Women
Brazilian Hips and Buttock Enlargement
Average Body Size MTF Transgender
Male and Female Skeleton Transsexuals
Treatment of Young Transsexuals
Puberty in Adolescents MTF Transgender
Treatment of Young MTF Transsexuals
Treatment of Intersex Infants
Androgen Insensitivity Syndrome
Female Physical Beauty Transgender
Transgender Female Beauty
Exercise, Fitness and Diet for Transsexual Women

Introduction
|
The natural purpose of the female human breast is to provide sustenance and nourishment to babies. While almost all transsexual women proudly regard their breasts as an important sign of their femininity and womanhood, few really consider their biological purpose.
|
Some years ago an English newspaper published a story about a young woman breast-feeding her baby in a restaurant, she was asked to leave and wasn't at all happy about that. Not really headline material, but readers then discovered that the woman in question was a male-to-female transsexual. As a 'husband', she had begun female hormone treatment at about the same time as his/her wife had become pregnant. After the baby's birth, the transwoman had acupuncture to help kick-in her own milk production and was sharing nursing duties with her former wife. The story was inevitably intended to be rather sensationalist, but some transsexual women reading it were probably surprised to learn that their breasts might be capable of performing the function that they were intended for by nature.
|

The breasts of a transsexual woman are in fact quite capable of producing milk ("lactation") given the following circumstances:
|
| The breast has not been badly damaged internally, e.g. by breast augmentation implants |
| The breast has a sufficiently well-developed internal structure |
| There are suitable stimuli (physical, hormonal, psychological) to start and then maintain the production of milk |
| There's a functional pituitary gland [Closely linked with point 3] |
| The woman is in reasonably good health - a sick or very poorly fed body won't waste energy and nutrition producing milk. |
Motivation
Inducing lactation is not easy; it will often take a lot of time and a lot of effort over a long period. The necessary motivation is essential or failure is almost inevitable.
|

One
study
of 27 genetic women who undertook a lactation induction program found that 24 (89 percent) were successfully breast feeding well-nourished children. All 11 women who had never previously lactated were successful.
|
Whilst quite such a high success rate cannot be achieved with male-to-female transsexual women, there's no doubt that given a high degree of motivation combined with medication, support, and encouragement; lactation induction can often be successful in transsexual women.
|
Breast Augmentation
A majority of transsexual women have had
breast augmentation
(implants), but the chances are good that the implants in themselves will not prevent lactation. Studies show that only about 10% of genetic XX woman with implants are unable to breast feed due to damage to their breasts caused by the implants. However, unfortunately many TS women have small and underdeveloped (hypo plastic) breasts prior to breast augmentation surgery. Although breast augmentation will greatly improve the external appearance of such breasts, even giving the impression of fully developed breasts, it does not solve the underlying milk supply problem due to insufficient internal development, and it will thus still be difficult for the woman to produce milk and nurse.
|

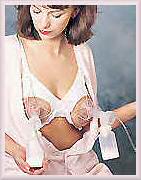
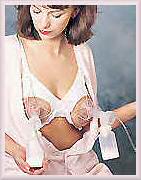
A transsexual woman expressing. Note the periareolar incision scars from breast augmentation.
|
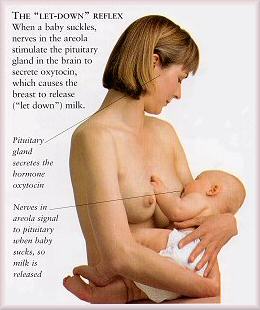
With a breast that has been surgically enlarged with implants, the nipple may be more or less sensitive than normal. If the nerves around the areola were not cut or damaged during the surgery then it should still be possible to nurse fully or partially. Nerves are vital to breastfeeding since they trigger the brain to release prolactin and oxytocin, two hormones that affect milk production. The chances of breastfeeding also improve if the milk duct system is intact. It's impossible to know the full extent of damage — if any — until a woman tries to make and express milk. Once lactation starts, implants may also cause exaggerated breast engorgement with more intense than normal pain, fever, and chills.
|
The likelihood that implants cause serious lactation and milk production problems depends directly upon the kind of surgery had. Incisions that were made under the fold of the breast (inframammary) or through the armpit (transaxillary ) shouldn't cause any trouble. However, the popular periareolar method, making a "smile" incision around the areola, has greater risk of problems.
|
There's absolutely no evidence that silicone from silicone implants leaks into breast milk, but even if it did, it probably wouldn't harm a baby. Silicone is very similar to a substance used to treat a baby's stomach gas.
|
Breast Development
|
In order to be able to produce milk internally the breast must have certain structures in place, but fortunately these are present at birth in every human, whether genetically male or female. It's also worth noting that highly visible factors such as breast size and areola diameter that are often of great importance to transsexual women in fact have relatively little effect on the breasts potential ability to lactate and the quantity and quality of the milk that will be produced. Whatever the size of her breasts, a M2F transsexual woman can still potentially breastfeed if the internal structures are in place and undamaged.
|
 Structure of the Female Breast
Structure of the Female Breast
Stages of Mammary Development
At birth the rudiments of the functional mammary gland are in place: the nipple and areola are formed along with a rudimentary system of mammary ducts extending into a small fat pad on the chest wall. The mammary gland remains a rudimentary system of small ducts until puberty when the advent of estrogen secretion by the ovaries brings about the first stage of the four stages of mammary development: mammogenesis, lactogenesis, lactation and involution.
|
Mammogenesis commences at puberty with the onset of estrogen secretion by the ovaries, usually between the ages of 10 and 12 in the girl. Estrogen causes enlargement of the mammary fat pad, one of the most estrogen-sensitive tissues in the human body, as well as lengthening and branching of the mammary ducts. About 40% of male children also initiate mammary development during puberty due to the tendency of the testis to secrete significant quantities of estrogens in early phases of its development. As testosterone secretion increases this function is lost.
|
Estrogen stimulates breast growth by acting on the mammary tissue. With the onset of the menstrual cycle the presence of progesterone stimulates the partial development of mammary alveoli, so that by the age of 20 the mammary gland in the woman who has not been pregnant consists of a fat pad through which course 10 to 15 long branching ducts, terminating in grape-like bunches of mammary alveoli. In the absence of pregnancy the gland maintains this structure until menopause.
|
Mammogenesis is completed during pregnancy, with the gland becoming able to secrete milk sometime after mid-pregnancy.
|
Lactogenesis (referred to as the time when the milk "comes in") starts about 40 hours after birth of the infant and is largely complete within five days.
|
When nursing has ceased the gland undergoes partial involution, losing many of its milk producing cells and structures, a process which is only completed after menopause.
|
Breast Development in the Transsexual Woman
A combination of supportive tissue, milk glands, and protective fat makes up a large portion of every woman's breasts (or mammary glands). Every person is born with milk ducts — a network of canals that transport milk through the breasts — present from birth. In the male-to-female transsexual woman the mammary glands stay quiet until commencing female hormone treatment releases a flood of estrogens in the body in what's effectively a female puberty - thus initiating the first phase of mammogenesis and causing the breasts to grow and swell.
|
The amount of hormone induced
breast development
achieved in the genetically XY male transsexual woman is very age dependent.
Young boy-to-girls
who start female treatment during their normal puberty years (i.e. about age 12-16) are likely to reach near normal breast development. But unfortunately the amount of development that can be expected rapidly tails off as the age of the commencement of hormone increases, and older transsexual women will commonly suffer from underdeveloped (hypo-plastic) breasts.
|
Breast development is categorized by the "Tanner Stages" scale which goes from I to V. It can again be emphasized that there is really NO minimum degree of breast development in order to be able to lactate; there are well documented instances of even men with minimal Tanner I breasts producing some milk and breast feeding without using hormones.

On the other hand there is no doubt that the higher the development stage, the easier it will usually be to start lactation and the greater the likely quantity of milk produced. In general, well developed Tanner IV or V type breasts are really required for successful nursing of a baby, perhaps a majority of the girls who start hormone treatment by age 25 are likely to achieve this but most older woman will achieve no more than Tanner III or even II breast development. Such hypo-plastic breasts are very small or narrow, lack normal fullness, and may seem bulbous or swollen at the tip. They are also likely to be widely spaced and one breast may be larger than the other. Hypo-plastic breasts don't develop and grow in response to any additional hormones given in order to simulate pregnancy and prepare the breast for lactation. Breasts of this kind have fewer milk glands than normal, leading to milk-production problems.
|
Breast Development During Pregnancy
|
It is necessary to understand how the human breast develops and prepares for milk production during a woman's pregnancy.
|
Mammogenesis is completed during pregnancy - indeed pregnancy is the period of greatest mammary growth. Extensive lobular and alveolar development occurs only during pregnancy, also milk secretory cells only develop during pregnancy, therefore this period is extremely important in determining the number of secretory cells in the lactating gland and the subsequent production of milk. Mammary growth (of the mother) accelerates throughout pregnancy and is fastest during the later stages of pregnancy, which coincides with the most rapid period of fetal growth.
|
Breast Structure of a Pregnant Woman
A pregnant woman will certainly notice a huge metamorphosis occurring in her bra cups. These physical changes include:
| darkened nipples and aureolas (the circle of skin surrounding the nipple) |
| the appearance of tiny bumps around the areola called the Glands of Montgomery |
But perhaps even more remarkable than this visible transformation are the extensive changes taking place inside her breasts, primarily under the stimulation of high levels of estrogen and progesterone, combined with the rising levels of prolactin from the pituitary and human placental lactogen (HPL) from the placenta.
|
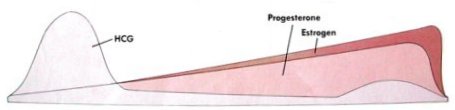 Progesterone and Estrogen blood plasma levels rise steadily during pregnancy.
Progesterone and Estrogen blood plasma levels rise steadily during pregnancy.
Nestled amid the breasts fat cells and glandular tissue is an intricate network of channels or canals called milk ducts. The additional hormones released during pregnancy cause the cells of the mammary fat pad to diminish in size and their place is taken by the developing ducts and alveoli.
|
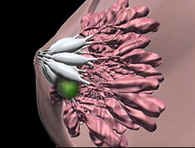
During the first three months of pregnancy the milk ducts increase in number and size; the ducts starting to branch off into smaller canals near the chest wall called ductules. During the mid-three months a cluster of small, grapelike, sacs called alveoli appear at the end of each ductule. A cluster of alveoli is called a lobule; a cluster of lobules is called a lobe. Each breast contains between 15 and 20 lobes, with one milk duct for every lobe. During the last three months of pregnancy the alveoli grow and mature.
|
Milk is produced inside the alveoli, which are surrounded by tiny muscles that squeeze the glands and push milk out into the ductules. Those ductules lead to a bigger duct that widens into a milk pool or milk sinus directly beneath the areola. Milk pools (also known as sinus) act as reservoirs that hold milk until a baby suckles it through tiny openings in the nipple. Essentially the 15 or 20 milk ducts act as individual straws that all end at the tip of the nipple and deliver milk into a baby's mouth.
|
|
The mammary gland becomes able to secrete milk sometime after mid-pregnancy, and begins to produce small amounts of a protein- and fat-rich secretion sometimes referred to as precolostrum. It seems likely that mammary development continues through the duration of pregnancy since milk secretion by mothers of premature infants often appears to be diminished. The onset of copious milk secretion (or lactogenesis) is held in check by the high levels of circulating progesterone until after child birth.
|
 A woman's breasts enlarge and the aureolas become darker
and more prominent during pregnancy
A woman's breasts enlarge and the aureolas become darker
and more prominent during pregnancy
Differentiation of the breast to its mature status occurs by the third month of pregnancy, although it will take about 6 months for the breast system to fully develop and become functional for lactation. Indeed, mammary growth will continue right up to birth, and even after if nursing. In a pregnant woman, by time the baby is born, glandular tissue has replaced most of the fat cells and accounts for the much enlarged breast. The increase in size varies greatly with the individual, ranging from zero to 800 cc of volume (and 1½ lb of weight!) per breast; the average being about 400 cc. It is normal for women to increase by one or two cup sizes during pregnancy, although this will decline (sometimes dramatically) after the cessation of lactation.
|
Oestrogen and Progesterone
Optimal mammary growth requires both estrogen and progesterone hormones. Together, these result in growth of the lobular and alveolar system. Both hormones are elevated during pregnancy, which is why there is no such "lobuloalveolar" growth during a woman's estrous (fertility) cycle, when only one of these hormones is elevated at a time. Progesterone is elevated throughout gestation (required for maintenance of pregnancy), while estrogen is particularly elevated during the second half of gestation. Consequently, most of the mammary growth during the first half of gestation is mainly ductal growth and lobular formation. In the second half of gestation, ductal growth continues, but most growth is lobuloalveolar.
|
Oestrogen and progesterone together establish the conditions needed for geometric cell multiplication to occur. For example, from one original cell, 8 cell divisions yields 128 cells.
During pregnancy, the mammary tissue has estrogen receptors and progesterone receptors. During lactation the mammary gland has estrogen receptors, but not progesterone receptors.
|
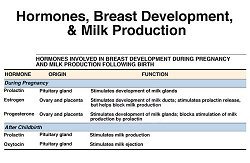
Other hormones
As well as the estrogen and progesterone hormones well known to transsexual women, there are several other hormones important to breast development and milk production. Indeed, mammary development in the pregnant woman takes place under the influence of an extraordinarily complex mix of hormones, including:- prolactin, human placental lactogen, estradiol (a type of estrogen), progesterone, insulin, cortisol, growth hormone, thyroid hormones ...
|
Prolactin is a protein hormone secreted from the anterior pituitary gland, as well as assisting in breast development; it stimulates and controls the actual production of milk.
|
In a pregnant woman, the placenta produces an important hormone called Human Placental Lactogen (HPL) which adjusts the maternal metabolism. One of its functions is similar to prolactin, i.e. stimulation of milk production by the mammary glands. HPL seems to work with estrogen and progesterone to increase the number of alveoli in mammary glands and also plays a role in making the alveoli functional (capable of producing milk). It's thought that the level of HPL hormone activity in the maternal blood regulates the extent of mammary development during late pregnancy. HPL also causes the secretion of a form of milk called colostrum from about the fifth month of pregnancy.
|
Yet another, and apparently unimportant, hormone is secreted by the pituitary gland of a pregnant woman, Melanocyte Stimulating Hormone (MSH). Its only known effect is to stimulate the skin to produce pigmentation, causing the aeroli to enlarge and darken.
|
Milk Production in a Maternal Mother
|
Lactogenesis
In a human mother lactogenesis, or the onset of copious milk secretion, (also referred to as the time when the milk "comes in") starts about 40-48 hours after child birth and is largely complete within five days. Milk secreted during the period between colostrum secretion and mature milk is called transition milk.
|
Lactogenesis is associated with an abrupt increase in milk volume secretion, which goes from a mean of about 50 ml per day on day 2 of lactation to about 500 ml per day on day 4. After this time there is a gradual volume increase to about 850 ml/day by three months postpartum. There are also profound changes in milk composition during the early post child birth period as the production of milk products comes into high gear. By 10 days after child birth the milk has assumed the composition characteristic of mature milk. There are minor composition changes that continue throughout lactation. Full lactation, or the secretion of mature milk, continues as long as the demand is there, up to three to four years for infants in some cultures.
|
Three factors are necessary for successful lactogenesis: a developed mammary gland, continued high plasma prolactin levels, and a fall in progesterone and estrogen levels that otherwise inhibit lactation - it can therefore be partially inhibited by high doses of estrogen. It is important to note that the milk "comes in" at the same rate whether the infant suckles during the first 48 hours or not. Thus the onset of milk secretion depends, not on milk removal from the breast, but on the changes in hormonal status associated with child birth. However, continued milk secretion depends on milk removal from the breast, the involutional process sets in after only 3 to 4 days if breast-feeding is not initiated.
|
Breast Stimulation in the Transsexual Woman
|
Hormonal Stimulation
Lacking the hormone producing ovaries and placenta present in a pregnant woman, the transsexual woman attempting to induce lactation must take estrogen by some artificial means (oral, injection, patches, etc.).
The estrogen is then abruptly withdrawn to mimic the rapid hormonal changes following delivery.
|

It is appropriate at this point to distinguish between trying to achieve some slight lactation, ranging from a few drops up to as much as 35% that of a nursing mother, and trying to achieve full and copious milk production as the primary source of nutrient for a baby. Both require some degree of hormonal stimulation, but it's a case of for how long, and also how well the breasts respond to the hormonal stimulation.
|
If only a minimal degree of lactation is being attempted then the high estrogen regimen may be as short as two weeks. But if full lactation is desired, then the transsexual woman must try to induce all the necessary developmental changes in her breasts by simulating a full period pregnancy by taking high doses of estrogen and progesterone hormones for a period of at least six months (probably not coincidently, a premature baby born after the 28th week or sixth month of pregnancy is "viable" and will often survive, and will thus require feeding). This sustained hormone treatment may stimulate her breast in to developing and preparing for lactation, but unfortunately transsexual women with underdeveloped hypo-plastic breasts are unlikely to succeed in this endeavor as their breasts will fail to respond to the additional hormones.
|
Also, in a pregnant woman her production of the estriol type of estrogen greatly increases and it becomes the dominant type of estrogen in her body. When present in high levels (unlike the non-pregnant lower levels), one of its effects is to help prepare the breast for milk production. However, the "weak" estriol estrogen is rarely taken by transsexual women as part of their hormone therapy, instead standard estrogen prescriptions are either of the estradiol (e.g. the Estrace brand) or estrone (e.g. the popular Premarin brand) types. Unfortunately, prolonged taking of large doses of these "strong" estrogen types, as is common with transsexual women, seems to desensitize the body to estriol, making stimulating the breast to prepare for lactation via hormones much more difficult.
|
Assuming that the hormones have an effect, the period of the most visible breast growth is often during the first eight weeks of treatment. This enlargement is potentially just temporary as it's primarily due to engorgement of the blood vessels, enabling increased circulation to the breasts. Thereafter, estrogen hormones stimulate cell mitosis and growth of the ductal system, the development and differentiation of the glandular tissue (lobules and alveoli) is dependent on progesterone, whilst breast fat accretion seems to require both.
|
Regarding other hormones found in pregnant woman:
| Prolactin may be produced naturally by the woman's pituitary gland which is helpful but probably insufficient. Currently, there is no prolactin medication on the market but prolactin-inducing |
drugs
are readily available and these can be taken to increase prolactin production to normal levels.
| HPL is valuable aid to breast development and lactation, but it's not naturally produced in the body of a transsexual woman. Highly purified HPL is available as a medication but unfortunately it's hard to obtain, very expensive (a course would cost several hundred dollars a day), and is very rarely used as a medication. |
| MSH is not believed to be necessary for lactation and is unlikely to be present in a transsexual woman. |

Hand-pumps are a very cheap mechanical aid to help stimulate lactation, but they are not suitable for prolonged heavy use.

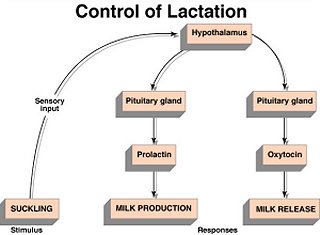
Mechanical Stimulation
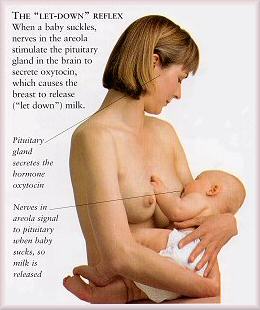
If it not possible to take additional female hormones in order to stimulate the breasts in to preparing for lactation, or if (as is commonly the case) the hormones have no effect due to hyperplasic breasts, all is still not lost. This is because prolactin and oxytocin, the hormones which govern lactation, are pituitary, not ovarian (or "female") hormones. Both prolactin, the milk-making hormone, and oxytocin, the milk-releasing hormone, are produced in response to nipple stimulation.
|
Most genetic women and some men can induce lactation to some extent with only mechanical stimulation. This consists of breast massage, nipple manipulation, and sucking - the later either by a baby or by expressing using a good quality electric
breast pump
with a double pump kit. Realistically expression by hand, or even with a hand pump, is simply not a practical alternative to an electric double breast pump given the frequent and prolonged sucking required on each breast.
|
A possibl
e expressing regime: Begin by expressing each breast for about five minutes, three times a day. Increase the length of the pumping session as you become more comfortable, until you are expressing for a total of about 15 to 20 minutes on each breast every two to three hours during the day. Expressing both breasts simultaneously by double-pumping obviously saves a lot of time every day by this point! You must include night time pumping sessions, allowing just one long 4-5 hours period of sleep.
|
Constant expressing will soon get to become hard work, when after a week you still haven't seen any milk at all, try not to become discouraged or concerned, unfortunately it may well take four to six weeks for the breasts to begin producing milk this way. Some dedicated women have reported only finally achieving some success after two or three months pumping!
|
Stress, tension, and fatigue all produce hormones that can reduce let-down. Avoid smoking and excessive alcohol and caffeine - these are known to inhibit a mother's milk production and let-down.
|
In order to pump effectively and increase milk supply it is essential to relax and stimulate as much as possible the milk let-down response crucial to milk expression. Suitable mental or environmental stimuli such as baby photo's, imagining yourself breast feeding, direct sucking stimulation of the nipples and immediately surrounding tissue, playing a tape of the cries of a hungry baby, ... etc, are essential aids to milk production. And a partner can greatly assist with sexually arousing mental stimulation and manual manipulation of the woman's body before, and even during, her expression period.
|
 Expressing by Hand
Expressing by Hand
 Breast massage - place one hand underneath your breast, the other on top. Slide the palm of one or both hands from the chest gently towards the nipple and apply mild pressure. Rotate your hands around the breast and repeat in order to reach all the milk ducts.
Breast massage - place one hand underneath your breast, the other on top. Slide the palm of one or both hands from the chest gently towards the nipple and apply mild pressure. Rotate your hands around the breast and repeat in order to reach all the milk ducts.
Expression Routine
It is essential to establish a routine to both start and then maintain lactation. For example begin by expressing each breast for about five minutes, three times a day. Increase the length of the pumping session as you become more comfortable, until you are expressing for a total of about 15 to 20 minutes on each breast every two to three hours during the day. Expressing both breasts simultaneously by double-pumping obviously saves a lot of time every day by this point! You must include night time pumping sessions, allowing just one long 4-5 hours period of sleep.
|
Here are some tips to help both manual and mechanical expression:
| Set up a regular milk expression schedule. |
| Allow enough time so you don't feel rushed. |
| Relax for 15 minutes before expressing, watch TV, listen to music, enjoy the occasional glass of wine. |
| Try to minimize distractions - take the phone off the hook, etc. |
| Try to express milk in a familiar and comfortable setting - privacy and comfortable seating promotes relaxation, which enhances let-down. |
| Follow a pre-expression routine: Use warmth to relax and stimulate milk flow by applying a warm compress to your breasts for 5 minutes or putting a warm wrap around your shoulders; relax with deep breathing and visualizations. |
| Encourage milk let-down by using an oxytocin nasal spray 2 or 3 minutes before using the breast pump - costly but worth it. |
| Think about babies - look at pictures of a baby and imagine him at your breast while you are expressing your milk. Play a tape of a hungry baby. |
| Before pumping stimulate your breasts and nipples through massage as illustrated right. |
| While pumping help "push" the milk towards the nipple - place your thumb opposite the fingers on either side of the areola (positioned as the pump allows), then rhythmically press your hand in towards your chest, gently squeezing the thumb and forefinger together. Rotate the fingers to get all the milk ducts. With practice you can do both breasts simultaneously. |
| Interrupt your pumping several times to pause and massage your breasts more. |
Achieving Milk Production in the Transsexual Woman
|
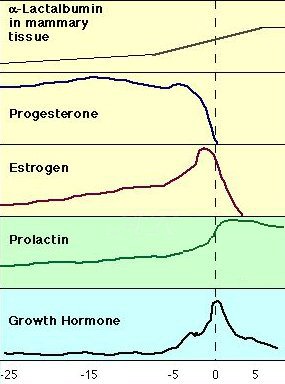 Relative changes in some of a mothers
hormone levels in the days around child birth. (The amount of a-lactalbumin in the mammary tissue is an indicator of lactogenesis.)
Relative changes in some of a mothers
hormone levels in the days around child birth. (The amount of a-lactalbumin in the mammary tissue is an indicator of lactogenesis.)
Lactogenesis
A genetic woman who's given birth also expels the hormone-producing placenta, and the estrogen and progesterone levels in her body suddenly drop. In a transsexual woman, ceasing an additional high estrogen and progesterone dosage that's been taken for several months will have the same affect if the hormones have worked. Recognizing that the "birth" has happened, the pituitary gland now signals the body to make lots of milk in order to nourish the baby by increasing its output of the hormone prolactin, and the changes in hormone levels thus cause milk production to begin. [Studies show that prolactin make a woman feel more "motherly", which is why some experts call it the mothering hormone!]
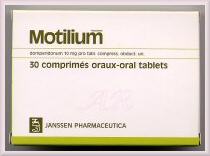
At this point mechanical breast stimulation, particularly sucking (with a breast pump or by a baby) should be started and an oxytocin nasal spray used to stimulate milk release. If not already begun a course of a
prolactin enhancing drug
such as domperidone (brand name Motilium is highly recommended to help milk production.
|
Success is not guaranteed, but some milk production can be expected in a majority of cases. Milk production typically begins between 1-4 weeks after initiating stimulation using prolactin enhancing drugs, although it can be as little as 2-3 days if hormones were taken and were effective, or as long as 4-6 weeks if relying purely on mechanical stimulation.
|
One study of induced lactation using enhancing medications describes the onset of milk production being between 5-13 days. At first, the woman may see only drops. During the time that milk production is building, women may notice changes in the colour of the nipples and areolar tissue. Breasts may become tender and fuller. Some women report increased thirst, and changes in their menstrual cycle or libido.

As the body readies itself for lactation, it pumps extra blood into the alveoli, making the breasts firm and full. Swollen blood vessels, combined with an abundance of milk, may make the breasts temporarily painful and engorged, but nursing or expressing frequently in the first few days will help relieve any discomfort.
|
Milk Release
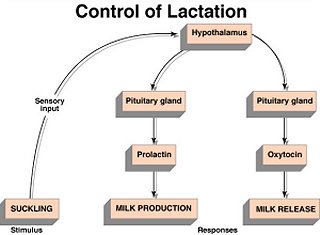
Obviously the best and most natural way to enhance let-down is by nursing a baby. As a baby sucks a nipple they stimulate the nursing mother's pituitary gland to release oxytocin (as well as prolactin) into her bloodstream. If a baby is not handy, the let-down reflex can also be encouraged by using an oxytocin nasal spray such as Syntocinon which can be prescribed by a doctor.
When oxytocin reaches the breast it causes the tiny muscles around the milk-filled alveoli to contract and squeeze. The milk is emptied into the ducts, which transport it to the milk pools just below the areola. When s/he suckles, the nursing infant presses the milk from the pools into his mouth, both manual and mechanical expression techniques can simulate this to a reasonable degree.
|
As the milk flow increases, the lactating woman may feel some tingling, stinging, burning, or prickling in her breasts. The milk may drip or even spray during let-down.
A benefit of oxytocin is that it the nursing woman may feel calm, satisfied, and even joyful as she nurses or expresses.
|
|
Maintaining Lactation
In order to maintain production it is necessary to frequently stimulate the milk-ejection reflex (MER) or "let-down" secretion, i.e. release milk from the internal alveoli.
|
The volume of milk produced is primarily a function of demand and is unaffected by maternal factors such as nutrition or age. Not a lot of milk will be produced unless suckling (natural or artificial) is frequent and consistent, the milk itself contains an inhibitor of milk production that builds up if the milk remains in the mammary gland for a prolonged period of time. Adequate milk removal from the breast is absolutely necessary for continued milk production.
|
If nursing an infant is not immediately and regularly possible then in order to maintain milk flow it will be necessary to artificially stimulate let-down by expression using a breast pump.
|
The more you nurse or express, the more milk that will be produced - nursing 10 to 15 minutes per breast every 2-3 hours (day and night!) is optimum! Expressing less than once every 5-8 hours, will result in dramatically less milk production, although some milk production will continue so long as an infant is suckled or milk is expressed at least twice per day. Less than that will result in complete cessation of milk production within one to three weeks. But with sufficient and regular stimulation, it is quite possible to maintain lactation for months, even years.
|

Two hormones are necessary for this continued production: oxytocin and prolactin. As mentioned above, oxytocin is necessary for the milk ejection reflex that extrudes milk from the alveolar lumen. Prolactin is necessary for continued milk production by the mammary alveoli. The secretion of both hormones is promoted by the afferent nerve impulses sent to the hypothalamus by the process of suckling. However, whereas the secretion of oxytocin is highly influenced by the activity of higher brain centers, prolactin secretion appears to be determined primarily by the strength and duration of the suckling stimulus. Although prolactin levels fall with prolonged lactation, at least some basal level appears to be necessary for continued milk production. There appears to be no direct relation between prolactin levels and milk production and therefore it is thought that the rate of milk production depends on control mechanisms localized within the mammary gland.

Transwoman Christine McGinn with one of the twins she is technically the father, but as a mother was able to breastfeed.

Breast Feeding by Transwomen
Achieving lactation is a challenge for MTF transsexuals (do you early want to wake up at 3:00 am to use a breast pump?), but it is quite possible as indicated at the start of this article for a transwoman to breast feed a baby. In 2010 the Oprah Winfrey program featured Dr Christine McGinn - the "Mum who fathered who own children". Christine is a lesbian MTF transsexual woman, before SRS she had a sperm sample frozen and this was used for an IVF procedure which happily resulted in her female partner giving birth to twins. Christine was able to breastfeed to the babies, she says:
|
"A lot of women who adopt go through a regimen of hormones before they have their child, and that enables them to breastfeed by the time they get their child. So I just did the same protocol. It's basically simulating pregnancy with hormones, and since I transitioned 10 years ago, I had enough breast development where it was basically the identical situation."
|
|
Is it worth it?
That of course depends upon yourself and your objectives. Hundreds of hours of effort, probably a considerable amount of money on pumps and drugs, and an enormous amount of will power is a non-trivial investment. I've had people email me to say that they have succeeded in getting fluid from their breasts, for some that seems to have been their sole objective and it may be enough for them. But in my mind, the lady in the newspaper article had the best objective ever possible - to breast feed her own baby. And here's some inspiring words from 29 year old XY, woman, newly married and with an adopted baby:
|

"[The baby] is wonderful and I was at his birth... I am breastfeeding him through induced lactation. With what I pumped and stored in advance he had only breast milk for one month.... now he has breast milk and formula. I feel great and life is very calm and lovely these days. Things in my life are so satisfying now. Now all I have to do is learn how to enjoy it!"
|
She followed the Ask Lenore
protocols
.
|
Additional Information
|
 Medela "Classic" pump
Medela "Classic" pump
Breast Pumps
If you don't have a baby or young child to nurse then hiring or buying a good quality, fully automated, electric breast pump that closely imitates the natural rate and rhythm of a baby's suck pattern is essential in order to regularly artificially stimulate let-down and express milk. Some automatic pumps can "double pump" (i.e. pump both breasts at once) thereby increasing prolactin levels and milk production while at the same time decreasing the amount of time a pumping session takes by about half to about 15 minutes.
|
 Medela Lactina
Medela Lactina
 Medela Pump in Style
Medela Pump in Style
A hand operated breast pump may initially seem a very attractive alternative to an electrical pump given that they can be bought for as little as $15, but it will usually be a big mistake to rely on this. Hand pumping each breast in turn, 6 or 7 times a day for 15 or 20 minutes, for perhaps several months is just not realistic for most people, even the manufacturers of these pumps only recommend them for occasional expression or relief.
|
A good quality electrical pump with a double pumping capability is simply essential. The best option is a hospital grade breast pump such as the "large"
Medela
(Classic) or the Ameda-Egnel Elite, unlike cheaper pumps these test and regulate pressure; they cost perhaps $40-$50 a month to rent. If you have problems finding a rental agent then try contacting the
LeLeche League
for help.
|
If you want to actually buy your pump, then a popular high-end option is the Medela Lactina at perhaps $500 (it can also often be rented for about $30-35 a month), while one entry level option is the Medela Pump-in-Style for around $300. Remember to get the double pump kit and accessories.
|

The popular but expensive Avent Isis manual breast pump costs about €/$45.
|
However it may be worth having a manual breast pump as well the electrical. The big advantage of a manual pump is that being light and small it can be conveniently carried in your bag when you know that you will be unable to meet a scheduled session on your electrical pump. If you are working, 30 minutes hidden in the toilets at lunch time using a hand pump may be the only option if the alternative is going more than about 6 hours without pumping. And a whole day without pumping might undo months of hard work and take you back to nearly the beginning! Because hand-pumps are cheap, it's possible to buy a couple of different models and experiment to find the one that is most comfortable, gives the best fit and suction to your breasts, is the most comfortable in the hand, and is the least tiring to use.
|
Lactation Enhancing Drugs
Prolactin and oxytocin, the hormones which actually govern lactation, are pituitary, not ovarian hormones (such as oestrogen). There are currently no human prolactin medications available, but Domperidone (brandname Motilium) is a drug which has, as a side effect, the increased production of the hormone prolactin by the pituitary gland, thus helping develop a more abundant milk supply faster as prolactin is the hormone which stimulates the cells in the mother's breast to produce milk. Another related but older medication is metoclopramide (brandnames Maxeran and Reglan), this is also known to increase milk production but it has frequent side effects which have made its use for many nursing mothers unacceptable (fatigue, irritability, depression). But in general Domperidone is much preferable; it has fewer side effects because it does not enter the brain tissue in significant amounts.
|
Genetic women trying to start lactation are advised that prolactin enhancing drugs need only be started only after the ending of any estrogen treatment as estrogen, particularly those types found in contraceptive pills, retard the start of lactation. However many transsexual women seem to gain considerable benefits from the breast developing effects of prolactin even if it's not initiating lactation because of their high estrogen intake, and thus should not be deterred from early use.
|
In many countries domperidone tablets are available without prescription. Generally, start at 20 milligram's (two 10 mg tablets) four times a day, i.e. about every 6 hours. After starting domperidone, it may take three or four days before any effect is noticed, though sometimes women notice an effect within 24 hours. It appears to take two to three weeks to get a maximum effect. Most women take the domperidone for 3 to 8 weeks, but women who are nursing adopted babies usually take the drug continuously in order to maintain lactation.
|
 Motilium 10mg tablets, produced by Janssen Pharmaceutica
Motilium 10mg tablets, produced by Janssen Pharmaceutica
Unfortunately Motilium is not yet available in the USA so domperidone may have to be used instead - usually just for 4 weeks rather than continuously. Also, in rare cases Motilum may cause stomach or digestive upsets and so domperidone may be preferred.
|
Some women find that herbal seed capsules such Blessed Thistle and Fenugreek help increase their lactation, and these are very commonly taken.
|
Hormone Regimen
I have been repeatedly asked for typical regimen for hormonal stimulation of the breast for lactation. I am not a medical practitioner, and there are many factors that must be taken in to account when determining the best regime and these must all be discussed with your doctor. As an
example only
, and derived from just limited evidence, the following daily regimen
may
be appropriate for a post-SRS woman under 40 years:
|
1 x Cyclogest 400 pessary from Cox Pharmaceuticals, containing 400mg Progesterone PhEur, daily
1 x Duphaston tablet from Solvat Pharmaceuticals, containing 10mg Dydrogesterone, twice daily
1 x Premarin tablet from Wyeth-Ayerst, containing 1.25mg Conjugated Estrogens, twice daily
1 or 2 or 3 Ovestin tablets from Organon, each containing 1 mg Estriol, 4 times daily (i.e. about every 6 hours)
1 or 2 or 3 Motilium tablets from Janssen, each containing 10 mg domperidone maleate, 4 times daily
A Syntocinon nasal spray from Sandoz Pharmaceuticals, containing oxytocin (use just before pumping or nursing to help elicit milk let-down)
also, 1 x 150mg Aspirin tablet, daily
|
Notes:
|
The regimen should be followed for at least 3 months, preferably 6 months, but no more than 9 months before attempted lactogensis.
|
The dosage of Ovestin and Motilium should be doubled to 2 tablets half way through the regimen.
|
The dosage of Ovestin and Motilium should be increased again to 3 tablets three days before attempted lactogensis.
|
Premarin is just one possible estrogen, if in any doubt stick with your normal estrogen proscription instead of Premarin, but add Ovestin or similar. The Premarin/Ovestin combination would be very unlikely if the woman has already been taking Premarin for a prolonged period. There is some anecdotal evidence that an Estradiol Valerate (e.g. Progynon-Depot from Schering) delivered by intramuscular injection may be an effective alternative to Premarin.
|
For a pre-SRS woman the dosages may need be much higher.
|
| Syntocinon and other oxytocin nasal spays may not be currently available in the USA. |
|
| Motilium may not be available in the USA. |
|
Ideally HPL should also be taken, but this is usually impractical as well as very costly.
|
Some "morning sickness" and nausea is very probable at first, if more severe side effects are experienced then medical help should be sought immediately. Long term use of such high dosage levels should be avoided, and if it's clear that no beneficial effects are occurring within 6-8 weeks then the regimen should be abandoned and the previous hormone regimen reverted to.
|
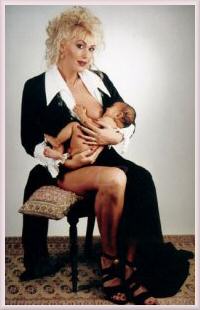 Transwoman Gloria Gray and baby Grace
Transwoman Gloria Gray and baby Grace
"Attempted lactogensis" means reverting to the prior hormonal regimen in order stimulate the start of milk production and lactation, this must involve a considerable reduction in estrogen and progesterone hormone intake, in pre-SRS women it may actually require a reduction to less than their normal regimen. If a baby is to be nursed then medical advice should be sought as to what hormones can still be safely taken and in what dosage, and any anti-androgens being taken
must
be stopped. Prolactin-enhancing drugs should continue to be taken, e.g. 2 Motilium tablets every 6 hours, each containing 10 mg domperidone maleate.
|
Antiandrogens may also be helpful to a pre-SRS transsexual women trying to induce lactation, although they should never be taken by a pregnant woman, or subsequently if breast feeding. The most commonly used anti-androgens are spironolactone (brand name Aldactone), flutamide (Eulexin) and cyproterone acetate (Androcur). Spironolactone, in a dosage of 25 to 100 mg administered twice daily, is the most commonly used antiandrogen because of its safety, availability and low cost. Flutamide is usually given in a dosage of 250 mg twice daily, and cyproterone is given in a dosage of 25 to 50 mg per day. Pre-SRS women may well already be taking much higher dosages of antiandrogens and these should not be increased - indeed in some cases it may be advisable to change the drug or reduce the dosage to the levels given here.
|
 Using a SNS
Using a SNS
Nutritional Value of Induced Milk
Milk released by a mother during the first few days of lactation after giving birth is called colostrum; it is richer in proteins, minerals, and immunoglobulins and is lower in calories and fat than the mature milk that develops over the following few weeks. The level of fats, lactose, and B vitamins gradually increases in breast milk during the first month of lactation. Mature breast milk is rich in the mother's white blood cells and hormones and substances such as immunoglobulins, which protect the infant against bacteria and other infectious agents.
|
The milk brought in by inducement skips the colostral phase, instead it more closely resembles transitional and mature breast milk. It is thus not ideal for new-born babies, but studies of non-maternal women nursing after induced lactation indicate that that their infants are well-nourished. However, it must be noted that many women felt they were only providing about 50-70% of the nutrition their babies needed with breast milk alone. If a transsexual woman is nursing it is therefore also very likely that she will be able to produce only a portion of the breast milk the baby needs, and it will be necessary to boost the baby's milk intake with formula. For this a Supplemental Nursing System (SNS) is valuable alternative to the traditional bottle. The device consists of a plastic pouch to hold breast milk or formula and attached thin, flexible tubes that run down each breast to the nipple. Since the baby takes both nipple and tube into his mouth when he suckles, he benefits from all the breast milk that is available.
|

Nursing
|
The female hormones taken by transsexual women induce breast development ranging from the slight to full. Typically their breasts are smaller than genetic women and about 50% of transsexual women have breast augmentations. However even very small breasts - particularly those of women who begin hormones before their 30's - can often function as nature intended, i.e. feed a baby.
Once the baby is born, the transsexual mother may well be able to experience the final physical act of pregnancy and birth and attempt to nurse her new baby - albeit with many assumptions such as being well enough after the delivery and her breasts are adequately developed and haven't been badly damaged by augmentation. There are already a few instances of transsexual women
lactating
and even breast feeding the babies of ex-wives or female partners.
Breastfeeding normally strongly recommended by doctors, it is by far and away the best and most convenient way to feed a baby. Not only will the baby be healthier, but it also helps the new mother lose weight more easily. Calories are burned during milk production; indeed some of the weight gained by a woman during pregnancy is intended to be used during lactation.
Breastfeeding also releases a hormone in the woman's body that acts as a natural tranquilizer, filling the mother with a sense of calm and well-being while she is breastfeeding.
Breast augmentation
, common in transsexual women, does not normally prevent breast feeding. The main reason that breastfeeding may not be recommended or encouraged by the physician is if the drugs and other hormones being taken by the mother may make the milk unsuitable for nursing.
It's very probable that the pregnancy and birth, and the associated hormone levels, will in itself be enough to induce lactation in the mother.
Summary
|
Inducing and maintaining lactation requires:
| During the pseudo pregnancy a high level of estrogen intake must be maintained for at least 6 months. Progesterone should also be taken as it plays a significant role in the development of lactating tissue (glands and ducts). |
| After the nominal birth, estrogen levels must drop dramatically to 'normal' levels'. In most transwomen this will kick the pituitary gland into releasing enough prolactin (the milk-producing hormone) to start some lactation. |
| Assuming that lactating tissue has developed and the milk comes in, it is then necessary to frequently nurse (or simulate nursing using a breast pump) in order to stimulate the milk "let-down" secretion (milk ejection) reflex - this is actually caused by the pituitary gland producing yet another hormone, oxytocin. |
| Maximum milk production requires regular suckling or pumping every 2-3 hours. Stimulation only every 5-8 hours will result in dramatically less milk production. Stimulation less frequent than that will result in the complete cessation of milk production some 1-3 weeks after it started. |
| If actual nursing of a baby is not immediately and regularly possible then in order to maintain milk flow it will be necessary to artificially encourage let-down, for example by: relaxing with a baby doll; hearing or thinking of a baby being hungry; stimulation of the nipples and immediately surrounding tissue. |
Useful Links
|

Good information on lactation and breast feeding can be found at the
BabyCenter
and the
International Lactation Consultant Association
|
La Leche League International
publishes the useful booklet "Nursing the Adopted Baby"
|
Information on lactation inducement can be found at
The Adoptive Breastfeeding Resource Website
|
Some very interesting information and protocols for induced lactation can be found at
Asklenore.info
|
Final Note: Feedback and additional contributions to this page are very welcome, your identity will
remain strictly confidential unless you state otherwise. I'm particularly interested in hearing from
trans-women who have experienced secretion or expression of colostrum or milk from their breasts.
|
|
Copyright (c) 2003, Annie Richards
Last updated: 28 February, 2003









 Structure of the Female Breast
Structure of the Female Breast
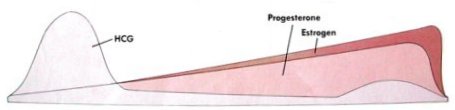 Progesterone and Estrogen blood plasma levels rise steadily during pregnancy.
Progesterone and Estrogen blood plasma levels rise steadily during pregnancy.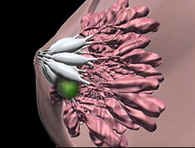
 A woman's breasts enlarge and the aureolas become darker
and more prominent during pregnancy
A woman's breasts enlarge and the aureolas become darker
and more prominent during pregnancy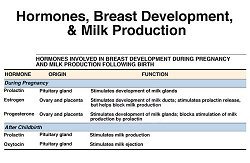



 Expressing by Hand
Expressing by Hand Breast massage - place one hand underneath your breast, the other on top. Slide the palm of one or both hands from the chest gently towards the nipple and apply mild pressure. Rotate your hands around the breast and repeat in order to reach all the milk ducts.
Breast massage - place one hand underneath your breast, the other on top. Slide the palm of one or both hands from the chest gently towards the nipple and apply mild pressure. Rotate your hands around the breast and repeat in order to reach all the milk ducts.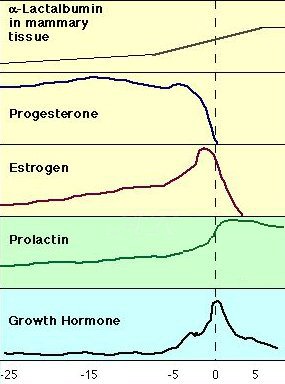 Relative changes in some of a mothers
hormone levels in the days around child birth. (The amount of a-lactalbumin in the mammary tissue is an indicator of lactogenesis.)
Relative changes in some of a mothers
hormone levels in the days around child birth. (The amount of a-lactalbumin in the mammary tissue is an indicator of lactogenesis.)




 Medela "Classic" pump
Medela "Classic" pump Medela Lactina
Medela Lactina Medela Pump in Style
Medela Pump in Style
 Motilium 10mg tablets, produced by Janssen Pharmaceutica
Motilium 10mg tablets, produced by Janssen Pharmaceutica Transwoman Gloria Gray and baby Grace
Transwoman Gloria Gray and baby Grace
 Using a SNS
Using a SNS